Niger becomes first African country to eliminate onchocerciasis

The World Health Organization (WHO) congratulates Niger for having met the criteria for onchocerciasis elimination, making it the fifth country globally and the first country in Africa to be acknowledged by WHO for interrupting transmission of the parasite Onchocerca volvulus.
Eliminating a disease is a significant achievement that requires tireless dedication. I congratulate Niger for its commitment to liberating its population from this blinding, stigmatizing illness that causes so much human suffering among the poorest. This success is yet another testament to the remarkable strides we have made against neglected tropical diseases and offers hope to other nations still battling onchocerciasis, demonstrating that elimination is possible.”
Dr. Tedros Adhanom Ghebreyesus, Who Director-General
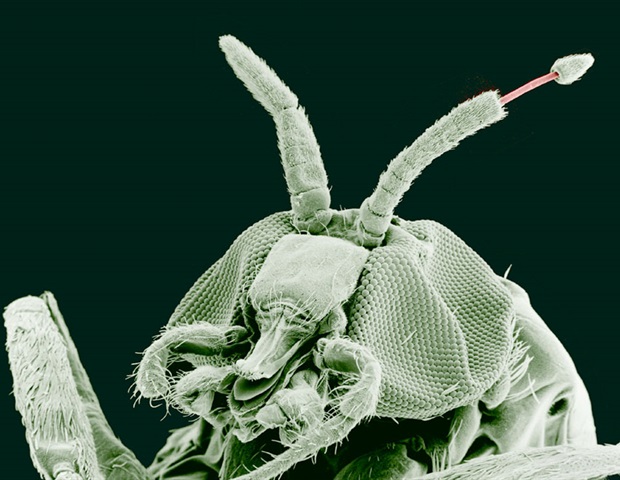
Onchocerciasis, commonly known as river blindness, is a parasitic disease and is the second leading infectious cause of blindness worldwide, after trachoma. It is transmitted to humans through the bites of infective black flies, primarily found in riverine areas. The disease primarily affects rural populations in sub-Saharan Africa and Yemen, with smaller endemic areas found in parts of Latin America.
Effective country-led efforts and partnerships
Between 1976 and 1989, under the umbrella of the WHO Onchocerciasis Control Programme in West Africa (OCP), Niger undertook vector control measures by spraying insecticides that significantly decreased levels of onchocerciasis transmission. Following the donation of ivermectin by Merck, Sharpe & Dohme (MSD), areas still affected by lymphatic filariasis (LF) underwent mass drug administration (MDA) with ivermectin and albendazole from 2008 to 2019, followed by surveillance. Since ivermectin is effective against both diseases, and areas targeted for LF MDA were also endemic for onchocerciasis, this intervention also contributed to interrupting the transmission of the Onchocerca volvulus parasite.
Niger started preliminary assessments on interruption of onchocerciasis transmission in 2014 after stopping LF MDA in most areas. This was followed by entomological and epidemiological surveys which revealed that the combination of medicine and vector control had successfully eliminated transmission of onchocerciasis, as evidenced by the reduction in prevalence from approximately 60% to 0.02%.
In addition to the vector control interventions and the medicines donated by MSD, a key factor contributing to Niger’s success is the partnership between the Nigerien government, WHO and nongovernmental organizations, which has helped mobilize resources and technical support. Continuous monitoring of the disease’s prevalence and its impact has enabled timely adjustments in strategies and ensured the effectiveness of interventions.
“Onchocerciasis has long caused immense human suffering. It has also impeded the economic development of affected communities, driving people away from rivers, which are often lifelines for livelihoods,” says Dr Matshidiso Moeti, WHO Regional Director for Africa. “Niger’s success ends this burden for its people. It also positions Niger as a model for the elimination of neglected tropical diseases in Africa. The country previously demonstrated its leadership in public health, by eliminating Guinea-worm disease in 2013. Today, it takes another historic step forward.”
Global progress
Globally, 54 countries have eliminated at least one neglected tropical disease.
Niger joins four other countries that have been verified by WHO for eliminating onchocerciasis, all in the Region of the Americas: Colombia (2013), Ecuador (2014), Guatemala (2016) and Mexico (2015).
In the WHO African Region, 21 countries have eliminated at least one neglected tropical disease. Onchocerciasis is the second neglected tropical disease eliminated in Niger: the country was certified free of dracunculiasis (Guinea-worm disease) transmission in 2013.
Source:

Sutherland century turns screw on wretched England in women’s Ashes | Women’s Ashes
After a mere 90-year wait, a second woman will finally join Peggy Antonio up on the Melbourne Cricket Ground honours board – take a bow, Annabel Sutherland. The 23-year-old already had a Test double-hundred to her name, scored against South Africa last year: now, she will go down in history as the first woman to ever score a hundred at the G.
By the close, Australia had extended their lead to 252, with the real possibility that Beth Mooney – unbeaten on 98 – will join Sutherland up on that honours board by Saturday evening.
This match has already broken the record for the largest attendance ever at a women’s Test, with an aggregate crowd of 23,561 across the first two days. And after the way England fielded on Friday, it now looks a near-certainty that another historical feat will be achieved before the weekend is over – the first 16-0 whitewash of the multi-format era.
England dropped eight catches, leaked piles of runs in the field, twice changed the pink ball (after Heather Knight complained that it was losing its shape), and barely looked like taking a wicket. Before play began, Ellyse Perry had been ruled fit to bat “if required”, after sustaining a hip injury in the field yesterday. But such is Australia’s batting depth that she never looked like being needed.
It was just after Australia levelled the scores – 20 minutes into the second session- that England’s wheels really came off. Oddly, it was also immediately after Sophie Ecclestone, who had bowled continually across the first session (17 consecutive overs), finally made a breakthrough, removing Alyssa Healy leg before.
But put yourself in Ecclestone’s shoes for a second. You’ve already bowled continually for the entire afternoon session, you’re England’s only frontline spinner, and you know there are two and a half more days of this to come. It’s the end of a fruitless tour, and you are exhausted. Then you turn around and see Mooney (who is averaging 61 this series) walking out to bat. Sutherland is at the other end: your team-mates have already dropped her twice, on 29 and 31, and now she has a century in her sights. Wouldn’t you be tempted to wave a white flag?
England did just that – Ecclestone, Lauren Filer and Ryana MacDonald-Gay beginning a competitive game of “who can produce the most tired misfield?” MacDonald-Gay put down a catch at cover off Ecclestone’s bowling; Ecclestone returned the favour by letting one slide through her hands at slip; Filer reached down to pick up the ball, let it through her legs, and back-kicked it halfway across the field.
The winner of the competition? A late entrant, Maia Bouchier, who put down an absolute sitter at gully. Mooney has refrained from publicly criticising England during this tour – asked on one occasion to explain how abjectly bad England have been, she replied, “those are your words, not mine” – but here her facial expressions did the talking: she shook her head in disbelief as England handed her a third life. If anything, it got worse after the dinner break: Ecclestone eventually put down a catch at slip which was so straightforward that Knight actually swapped her out of the cordon.
after newsletter promotion
In among it all, Sutherland calmly made her way to a third Test century, joyously raising her bat to the crowd’s standing ovation, and lapping up another one after MacDonald-Gay finally bowled her through the gate for 163, with job firmly done. It’s rare that a side can manage to throw away a Test match in a single session, but give it 24 hours and England will be able to add that one to their CV.

New study challenges link between mother’s health during pregnancy and autism risk

While many studies have reported a link between a mother’s health condition during pregnancy and her child’s risk of autism, a new study shows that nearly all of these “associations” can otherwise be explained by factors such as genetics, exposure to pollution, and access to healthcare.
Led by researchers at NYU Langone Health, the study revealed that, of the few conditions truly associated with autism, all were actually complications with the fetus – leading the authors to believe that those symptoms were early signs of autism in the child and not the cause of it.
“Our study shows that there is no convincing evidence that any of these other diagnoses in the mother can cause autism,” said study senior author Magdalena Janecka, PhD, an associate professor in the Department of Child and Adolescent Psychiatry and in the Department of Population Health, at NYU Grossman School of Medicine.
Publishing in the journal Nature Medicine online Jan. 31, the new study included an analysis of
the medical histories of more than 1.1 million pregnancies (among 600,000 mothers) from a national registry in Denmark. Unlike medical records in the United States, which are often scattered among many different medical providers an individual sees during their lifetime, in Denmark all of an individual’s health records are consolidated under a single government-issued number, which enabled researchers to check each woman for more than 1,700 distinct diagnoses as defined by international standards, known as ICD-10 codes. From these, researchers focused their analysis on those diagnosed in at least 0.1% of pregnancies (236 diagnoses).
We believe our study is the first to comprehensively examine the entire medical history of the mother and explore a wide range of possible associations, controlling for multiple concurrent conditions and confounding factors.”
Vahe Khachadourian, MD, PhD, MPH, study lead author, research assistant professor in the Department of Child and Adolescent Psychiatry at NYU Grossman School of Medicine
Denmark has strict safeguards in place to prevent misuse of the registry data, says Janecka, since it contains personal information. But because of the individual-specific information, the researchers were able to cross-check every diagnosis a woman had had with her children’s risk of autism.
For the study, the researchers corrected for factors that could confound, or offer an alternative explanation for, the link between the diagnosis a woman received and a child’s autism diagnosis. These factors include sociodemographic status and the mother’s age during pregnancy, since children of older mothers are more likely to be diagnosed with autism, and their mothers are also more likely to receive certain diagnoses, such as hypertension, than their younger counterparts.
After accounting for these confounding factors, as well as for concurrent diagnoses, 30 were still statistically associated with autism in the child. To determine if these happened to occur alongside rather than cause autism, the researchers then included the siblings of autistic children in the analysis. If a mother was diagnosed with the same condition during pregnancies of children with and without autism, then it would suggest that factors other than her diagnosis were influencing the link with autism. This step disentangled the conditions that could be attributable to familial factors, such as genetics and environmental exposure to pollution, from those that may be causing autism.
Genetics is a strong familial confounder (plausible explanation) for autism, the researchers say. Certain genes that increase the risk of someone having depression are also more closely tied to them having autism. If a woman suffers a bout of depression during pregnancy and her child is autistic, it is much more likely that mother and child share genes that cause both conditions, rather than that the chemical effects of depression somehow affected the fetus to cause autism during development.
Researchers also analyzed fathers’ medical histories. Any association between a paternal diagnosis and autism would most likely be caused by familial factors, since the father’s direct effects on a fetus postconception are likely very limited. In fact, the researchers observed that a lot of paternal diagnoses are just as related to child autism as the maternal diagnoses.
After accounting for the familial factors, the only maternal diagnosis that was still strongly statistically associated with autism was pregnancy complications related to the fetus.
“Our interpretation is that these fetal diagnoses likely do not cause autism, but are instead early signs of it,” said Janecka. “The predominant hypothesis is that autism really starts prenatally. Even before a child receives a diagnosis for autism, developmental changes have been happening the entire time.
“Many mothers of children with autism feel guilty about it,” said Janecka, “thinking that they did something wrong during pregnancy, and it is heartbreaking. I think showing that these things are not going to cause autism is important and may lead to more effective ways to support autistic children and their families.”
Autism is recognized as a developmental disorder that often appears in childhood and is marked by a range of difficulties with social interactions and repetitive behaviors. Symptoms vary widely into adulthood but can include reduced eye contact, reluctance to engage in playtime activities, repeating gestures or sounds, and an indifference to temperature extremes. According to federal estimates, one in every 54 children in the United States is affected by autism.
Funding support for the study was provided by National Institutes of Health grants R01MH124817 and T32MH122394, Lundbeck Foundation grants R102-A9118 and R155- 2014-1724, the Seaver Foundation, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development grant HD098883.
Other Study Co-Investigators Are Elias Speltskov, Jakob Grove, and Stefan Nygaard Hansen at Aarhus University in Denmark; Paul O’reilly, Joseph Buxbaum, Abraham Reichenberg, and Sven Sandin at Icahn School of Medicine at Mount Sinai in New York City; Lisa Croen at Kaser Permanent Northern California in Oakland; And Diana schhendel at Drexel University in Philadelphia.
Source:
Journal reference:
Khachadourian, V., et al. (2025) Familial confounding in the associations between maternal health and autism. Nature Medicine. doi.org/10.1038/s41591-024-03479-5.

Testing your seeds now will save you time, effort and waste in your garden come spring | Gardening advice
I like to think of myself as an organised person, but if you met my seed box, you may disagree. It’s a recycled shoe box that once housed wellies, with cardboard dividing it into compartments labelled by plant family. Each section is a chaos of packets, envelopes, little jars and paper folded around seeds that have been bought, shared and saved. Not everything is labelled, some packets are empty and many of the seeds have been hanging around for too many years to still be fertile.
Seeds don’t last for ever, unfortunately. Their viability varies depending on how long they have been stored, the conditions they have been stored in and the type of seed – onion seeds, for example, are best sown within a year or two, whereas cucumber and kale seeds can be stored for about five years. Generally speaking, a seed will last longer when it is kept in the opposite conditions to those required for germination. For most seeds, this means keeping them cool and dry.
During this quieter time of year, with the sowing season soon to come, conducting seed viability tests is a worthwhile and timely task that can help you determine whether to sow the older seeds you already have or buy new ones. It’s a relatively straightforward process.
Take the seed that you’d like to test and sprinkle a sample on a piece of dampened kitchen towel. Larger seeds – such as peas and beans – are worth soaking first. Then put your dampened seeds on a plate and pop them either into a freezer bag or a plastic container before placing them somewhere warm. If you’re testing multiple seeds at the same time, it’s essential that you’re diligent with your labelling as it’s incredibly easy to forget what’s what once you’ve left them to (hopefully) germinate.
Check your seeds every few days for signs of sprouting, making sure that the paper is kept moist but not saturated (which will cause your seeds to rot before they have a chance to emerge). After about two weeks, all the seeds that are viable ought to have germinated. You’ll want to see some seed leaf and root development.
Ideally, all the seeds will have germinated, which would make their germination rate 100%, but for older seeds it’s likely that the rate will be lower. If half of your seed sample show signs of life, they’ve got a 50% germination rate so it’s a good idea to sow twice as many seeds as you would with fresh seed to get the results that your planting plan calls for.
after newsletter promotion
Sowing into a tray then pricking out the seedlings that do appear is another way to use low viability seed. Anything lower than 50% is probably not worth your effort, the compost they’d use or seed tray space they’d take up.

Drawn-out overhaul of troubled Montana hospital leaves lawmakers in limbo
Montana lawmakers are grappling with what they can do to improve patient care and operations at the state’s psychiatric hospital since realizing that the efforts underway to restore the troubled facility’s good standing could take more time.
The nearly 150-year-old Montana State Hospital has recently struggled to care for patients and retain staff. The problems came to a head in 2022, when federal investigators yanked the hospital’s federal certification — and funding — from the Centers for Medicare & Medicaid Services because of a pattern of patient deaths found to be preventable, as well as injuries and falls.
Since then, Republican Gov. Greg Gianforte’s administration has launched a complex and expensive overhaul of the Montana State Hospital’s operations with the goal of regaining certification. That outcome may require years more work and tens of millions in additional funding from the Republican-majority legislature.
At least some lawmakers begrudgingly acknowledge the protracted scenario, reflecting on the time spent trying to pressure the state health department to move at a faster pace.
“I think it’s going to be done when it’s done,” said Republican Sen. Dennis Lenz, a longtime lawmaker who sits on the health department’s budget committee in the state legislature. “It’s like telling your teenager, ‘Come on, get your act together. Come on, put your clothes away.'”
Lawmakers in this session have the power to add or restrict money for Gianforte’s health department and write laws related to state hospital oversight, admissions, and discharge processes.
Health officials in the Gianforte administration are neck-deep in efforts to renovate the facility, slow its revolving door of leaders, and increase staff retention. Lawmakers are instead turning their attention toward ways to strengthen mental health services outside the hospital — an effort urged on by other mental health care advocates.
“I think the future of the hospital, and whether or not it will improve enough to be considered meeting the minimum federal standards for a hospital, rests on whether or not Montana can build up its community-based services,” said David Carlson, executive director of Disability Rights Montana, a federally appointed watchdog group that advocates for patients in state facilities. “They’re so interlinked. And we’re putting too much pressure on a singular hospital in Warm Springs.”
The state hospital’s campus, located in southwestern Montana near Butte, treats criminally and civilly committed patients. Inspectors decided to decertify the hospital after identifying numerous violations of patient care standards, including deaths, infection control issues related to covid-19, repeated falls, and medication mismanagement that amounted to “chemical restraints.”
In the wake of that loss, the hospital’s top-level leadership has rotated through five administrators. Medical staffers have strongly criticized new mandates and changing protocols. The facility relies on expensive contracted health professionals, and, until this month, a consulting firm to oversee the hospital’s operations. Waitlists for the unit of criminally charged patients are persistently long, bogging down court cases and leaving suspects incarcerated in jails throughout the state.
In mid-January presentations to lawmakers, state health officials gave mixed reviews about how the hospital is improving.
The facility has discontinued the use of chemical restraints entirely, officials said, and recently hired a permanent CEO and chief medical officer. Doug Harrington, Montana’s state medical officer, said the facility is also seeing more interest from prospective employees applying for open positions.
“The short answer is yes, things are changing. And it will take time; it’s not going to happen overnight. But the seeds have already been planted, and we’re seeing some of the fruit growing up,” Harrington told lawmakers on the health department’s budget subcommittee.
Harrington also acknowledged that the timeline for regaining certification from CMS was pushed back to 2026 due to physical repairs at the central hospital.
“When you start tearing the wall out, you frequently find fungus, black mold, infectious agents in the water of the cooling systems,” he said. “We need to shut down an entire wing and move those patients somewhere else so that that can be sealed off and worked on.”
Last fall, the state began moving patients to a 20-bed space in Helena leased from Shodair Children’s Hospital to allow for the renovation of one of the hospital’s wings.
In total, the Gianforte administration has requested that the legislature greenlight a one-time allocation of almost $61.5 million to continue to cover the cost of contracting clinical and nursing staff at the state hospital. The facility’s two-year budget, including that request, is more than $167 million.
Another high-priority upgrade for the hospital is the creation of a comprehensive electronic health records system.
Funding for that project — approximately $27.6 million to cover all state facilities — was originally approved by the legislature in 2023. But state officials have yet to ink a contract for the electronic system, and they say the cost could change during negotiations with a future vendor.
The state estimated in January that the electronic records project, from development to implementation, would take three years. A spokesperson for the hospital said the department expects to have a contract signed and to begin that timeline in March.
Previous efforts to legislate change at the hospital are still in motion. Lawmakers passed a bill with bipartisan support in 2023 that directed the state to move patients with a primary diagnosis of dementia, such as Alzheimer’s disease, or a traumatic brain injury out of the hospital and into community-based facilities better equipped to care for patients with memory issues and other cognitive disabilities.
The bill set a deadline for those patients to be moved by the end of this June. Jennifer Carlson, a former Republican lawmaker who chairs a committee to oversee that transition, said the department still has patients in residence who are subject to the legislation, but she’s feeling optimistic about meeting that target.
Another bill from 2023 required the state health department to share unredacted abuse and neglect reports with Disability Rights Montana, the designated federal civil rights inspector. But since the law took effect, staff turnover and changing protocols at the hospital made for inconsistent application of the law, officials with the advocacy group said.
David Carlson of Disability Rights Montana, who is not related to Jennifer Carlson, said lawmakers’ and advocates’ time may be better spent this session on trying to reduce the number of patients that hospital staffers are struggling to care for. One strategy is to finalize the transfer of memory-care patients targeted by the 2023 law to community-based facilities, he said, and help grow local mental health crisis services.
Even with those changes, he added, the responsibility for high-quality patient care rests with the Gianforte administration and the hospital’s leadership team.
Ultimately, if medical standards and internal protocols don’t improve, David Carlson said, the last branch of government that can put a check on the hospital’s operations is the judiciary. Disability Rights Montana has previously represented patients suing state institutions over civil rights violations and errors in patient care.
“That’s not a threat. That’s just a description of how this all works,” Carlson said. “Accountability will come from some branch of government. The administration can embrace it themselves and get ahead of it. The legislature can lay it on there, or we can have the courts do it.”

Chelsea join the race to sign striker Evan Ferguson from Brighton | Chelsea
Chelsea have joined the race to sign the Brighton striker Evan Ferguson. Brighton are willing to sell or loan the Republic of Ireland international, who has been the subject of interest from Arsenal, Bayer Leverkusen, Bournemouth, Everton Tottenham and West Ham.
Leverkusen were seen as frontrunners for Ferguson only for their plans to be complicated by Al-Nassr pulling out of a deal to sign Victor Boniface. That left West Ham in a strong position but they risk being outmuscled by Chelsea. Enzo Maresca is keen to bring in a striker to compete with Nicolas Jackson, who has gone seven games without scoring in the Premier League, and Ferguson is well known to the Stamford Bridge club’s recruitment team. Paul Winstanley, Chelsea’s co-sporting director, was previously at Brighton.
It is unclear if Chelsea, who have recruited heavily from Brighton during the past two-and-a-half years, want a loan or a permanent deal. It is thought Ferguson, who is recovering from an ankle injury, could be available for £40m. The 20-year-old has scored once this season but is seen as one of the best young forwards in England.
The race for Ferguson is unpredictable. Arsenal need a striker but do not have any domestic loans left and have targeted Aston Villa’s Ollie Watkins. Ferguson would be below Richarlison and Dominic Solanke in the pecking order at Spurs. He would have opportunities to play regularly at Bournemouth, however, who have lost Enes Unal and Evanilson to injury, as well as at West Ham.
Chelsea have alternative options before the transfer window closes on Monday. They remain interested in the Bayern Munich forward Mathys Tel and the Manchester United winger Alejandro Garnacho. Spurs are pushing to sign Tel after holding talks with Bayern but there are doubts over whether they have the funds to complete a deal for the Frenchman.
Other targets for Chelsea include Athletic Bilbao’s Nico Williams and Borussia Dortmund’s Jamie Bynoe-Gittens. They are also tracking the Ipswich forward Liam Delap. Villa, meanwhile, are looking to sign the France defender Axel Disasi and the Portugal forward João Félix from Chelsea, who have agreed a deal for their academy product Harvey Vale to join Queens Park Rangers on a free transfer.

A novel AI-driven tool to streamline tuberculosis evaluation in hospitals
A new clinical decision support system, “TBorNotTB,” helps streamline airborne infection isolation decisions, reducing workload while maintaining TB detection accuracy.
 Study: TB or not TB? Development and validation of a clinical decision support system to inform airborne isolation requirements in the evaluation of suspected tuberculosis. Image Credit: SewCreamStudio/Shutterstock.com
Study: TB or not TB? Development and validation of a clinical decision support system to inform airborne isolation requirements in the evaluation of suspected tuberculosis. Image Credit: SewCreamStudio/Shutterstock.com
In a recent study published in Infection Control and Hospital Epidemiologyresearchers presented a clinical decision support system (CDSS) to guide the evaluation of suspected tuberculosis (TB).
Background
In the United States (US), TB incidence has reduced from 10.4 cases per 100,000 people in 1992 to 2.2 cases per 100,000 in 2020, with nosocomial transmission being rare in recent years.
Nevertheless, TB incidence surged to 2.9 per 100,000 people in the US in 2023. Meanwhile, hospitals face capacity and staffing challenges, rendering decision-making for suspected TB patients more urgent.
Current guidelines for suspected TB recommend testing sputum samples for mycobacterial culture and acid-fast bacilli (AFB) smear, with airborne infection isolation (AII) implemented.
Nevertheless, cultures usually take ≥ two weeks, and nearly half of individuals with pulmonary TB show negative smears. While nucleic acid amplification tests (NAATs) have greater sensitivity than AFB smears, they are significantly less sensitive than culture.
As such, discontinuing NAATs and smear results would be premature and risk transmission to healthcare workers and other patients. Therefore, infection prevention and control (IPC) personnel often perform an additional review of patient records before aII discontinuation.
In addition, discussions with relevant consultants and the primary team may follow to ascertain whether TB is unlikely to favor AII discontinuation, which is time- and labor-intensive.
About the study
The study aimed to develop a clinical decision support system (CDSS) to assist in discontinuing airborne infection isolation (AII) while ensuring appropriate evaluation of suspected tuberculosis (TB) cases. Researchers created the “TBorNotTB” system to streamline AII discontinuation without compromising care for patients with possible TB who test negative on nucleic acid amplification tests (NAAT) and acid-fast bacilli (AFB) smears.
A panel of experts designed and refined a set of questions based on clinical guidelines and epidemiologic data using the Delphi consensus method. These questions were tested on hospitalized patients at Massachusetts General Hospital (MGH).
The CDSS assigned scores based on epidemiologic risk factors, TB symptoms, medical history, bronchoscopy/sputum results, and chest imaging. If a patient’s score exceeded a set threshold, AII was automatically discontinued; otherwise, further evaluation was recommended.
To validate the CDSS, researchers conducted a case-control analysis using data from the Mass General Brigham (MGB) system. The tool was retrospectively applied to patients with culture-confirmed TB (cases) and matched culture-negative controls.
Variables that did not improve predictive accuracy were removed or down-weighted. The model’s performance was then fine-tuned by adjusting the weight of key TB predictors and analyzing its sensitivity, specificity, and area under the curve (AUC).
A sub-group analysis compared the CDSS’s effectiveness before and after the COVID-19 pandemic. Additionally, the study estimated the total infection prevention and control (IPC) person-hours saved at MGH annually through the CDSS implementation.
Finally, the study suggests that TB is unlikely to be a strong driver for AII discontinuation, given the time and labor-intensive nature of the process.
Findings
The researchers identified multiple predictors of TB in the case-control sub-study. Cavitary lesions or other findings suspicious of TB on the chest radiology report were strongly associated with active TB.
Further, prior residence in a country highly endemic for TB was the strongest epidemiologic risk factor for TB. A history of positive interferon-γ release assay (IGRA) was also a strong predictor of active TB.
Notably, a negative IGRA or tubulin skin test within the past month showed a negative association with TB. A history of conditions deemed to elevate TB risk was not associated with TB.
A history of weight loss was the only traditional TB symptom that predicted active TB. Further, marked improvement or resolution of symptoms with treatment for alternative diagnosis showed a strong negative association with TB.
This initial CDSS model showed 16% specificity and 100% sensitivity. Following iterative revisions to the scoring system, the final model showed a sensitivity of 100%, specificity of 27%, and AUC of 0.87.
There were no differences in model performance pre- and post-COVID-19. The researchers estimated that TBorNotTB could save more than 40 IPC person-hours annually at MGH.
Conclusions
Together, the study developed and validated a novel CDSS to guide the diagnostic evaluation of patients with suspected TB in low-prevalence settings. Prior positive IGRA, residence in a TB-endemic country, and chest radiological findings suspicious of TB were significant predictors of TB.
The final CDSS model showed modest specificity and high sensitivity in detecting TB. Overall, TBorNotTB could help reduce the risk of nosocomial transmission and save considerable IPC person-time.

Pressure grows on Met over ‘heavy-handed’ policing of pro-Gaza protest | Metropolitan police
The Met police is facing growing questions over its handling of a pro-Palestine protest in central London at which more than 70 people were arrested.
On Friday, trade union leaders became the latest group to write to the home secretary, Yvette Cooperdemanding an independent inquiry into “repressive and heavy-handed policing” at the 18 January demonstration.
Their letter followed others by legal experts, MPs and peers and the British Palestinian Committeeto Cooper making the same demand and also calling for a review of legislation limiting protest, brought in by the Conservative government.
Amnesty International has also expressed concerns about the policing, while the Green party London Assembly member Zoë Garbett told the assembly’s police and crime committee meeting that she had been contacted by more than 150 people who described incidents of kettling and police violence towards children, pregnant women and older people.
In a statement after the demonstration, commander Adam Slonecki, who led the policing operation, said there was “a deliberate effort, including by protest organisers, to breach conditions and attempt to march out of Whitehall”. He described it as “a serious escalation in criminality”.
Previous marches, which have taken place since Israel launched its assault on Gaza after the 7 October 2023 attack by Hamas, have passed largely without incident and relations between police and the organisers, Palestine Solidarity Campaign (PSC), had been considered cordial.
But restrictions placed on the route of the latest rally preventing a march to the BBC’s headquarters, along with the number of arrests – including of the PSC director, Ben Jamal, and the rally’s chief steward, Chris Nineham, of the Stop the War coalition – have soured relations.
Jamal and Nineham have been charged with public order offences, while 60 of the 77 people arrested were said to have breached the conditions imposed, which the Met said was to protect a synagogue near to the BBC offices.
The force said the 60 people broke through police lines, but the organisers and marchers, including the Green party deputy leader, Zack Polanski, have said protesters were arrested without warning for inadvertently being outside the ill-defined permitted area.
Polanski told the Guardian columnist Owen Jones that he intervened when police tried to prevent a woman in her late 60s or early 70s from leaving the rally area to go to the toilet, while a Stop the War steward alleged they prevented officers arresting a 13-year-old girl with a placard for being in breach of the Public Order Act because she arrived before the allowed assembly time.
The various letters say the Met falsely accused protesters carrying flowers – including the former Labour leader Jeremy Corbyn and his shadow chancellor, John McDonnell – of forcing their way through police lines when video footage shows they were initially waved through by officers.
The trade union leaders from, among others, the Public and Commercial Services Union (PCSU), the Communication Workers Union (CWU), the University and College Union, and the transport unions RMT, TSSA and Aslef, say: “As trade unionists we are only too aware how heavy-handed policing, followed by the construction of false media narratives, have often served as a pretext to undermine our democratic rights to demonstrate and take industrial action.
“We are also conscious that the repressive powers used by the police on Saturday stem from efforts by the previous Conservative government to curb our freedom to strike as well as protest.”
The British-Egyptian actor Khalid Abdalla, star of The Crown and The Day of the Jackal, said the policing was reminiscent of policing he had seen in Egypt.
With the next march announced for 15 February, the policing response – before and on the day – is certain to come under added scrutiny.
Trump’s order on gender-affirming care escalates reversal of trans rights
President Donald Trump ratcheted up his administration’s reversal of transgender rights on Tuesday with an executive order that seeks to intervene in parents’ medical decisions by prohibiting government-funded insurance coverage of puberty blockers or surgery for people under 19.
Trump’s order, titled “Protecting Children From Chemical and Surgical Mutilation,” is certain to face legal challenges and would require congressional or regulatory actions to be fully enacted. But transgender people and their advocates are concerned it will nonetheless discourage prescriptions and medical procedures they consider to be lifesaving in some cases, while complicating insurance coverage for gender-affirming care.
“It can’t be understated how harmful this executive order is, even though it doesn’t do anything on its own,” said Andrew Ortiz, a senior policy attorney at the Transgender Law Center. “It shows where the administration wants to go, where it wants the agencies to put their efforts and energies.”
The order is one of several Trump has issued, less than two weeks since taking office, that target the trans community. He has directed his administration to recognize only the male and female sex — and to abandon the term “gender” altogether. He ordered the State Department to issue passports identifying Americans only by their genders assigned at birth. He has encouraged the Justice Department to prosecute teachers and other school officials who help trans children transition, including by using their preferred names. And he signed an order that’s expected to lead to transgender people being banned from military service.
“We’re terrified. We cry every day. Hurting my family and my kid is winning politics for Republicans right now,” said the parent of a transgender child who lives in Missouri and asked not to be identified for fear of being targeted. “Every bone in my body is telling me I can’t keep my child safe from my government anymore, I can’t keep my family safe.”
About 300,000 American children ages 13-17 identify as transgender, according to the Williams Institute at the UCLA School of Law, which researches sexual orientation and gender identity law and public policy. But the number who seek gender-affirming care is believed to be far fewer. An examination by Reuters and Komodo Health of about 330 million health insurance claims filed from 2017 to 2021 found that fewer than 15,000 patients ages 6 to 17 with a diagnosis of gender dysphoria had received gender-affirming hormone therapy and fewer than 5,000 had started puberty-blocking medications — though the annual number of such patients more than doubled over the five-year span.
Trump’s order seeking to disrupt insurance coverage for young people, the Williams Institute said in a brief, “will likely at least limit the availability of gender-affirming care or make it more difficult to access in the short term and could increase risk for both providers and recipients of the care.”
Much of what the order calls for would require rule changes or other federal guidance, which can take weeks to months. Though it is mostly directed toward government health insurance programs, the order could have private-sector implications, too, and is likely to face litigation from states or advocacy organizations.
Specifically, the directive intends to limit insurance coverage for hormonal or surgical treatments that help young people transition.
It directs the secretary of the Department of Health and Human Services to “take all appropriate steps” to end insurance coverage of such treatments. It specifically names several government programs such as Tricare, which serves the military and its dependents; Medicare and Medicaid; federal and postal health benefit programs; and the Foreign Service Benefit Plan.
“The aim here is clearly targeted at federally funded plans, such as Medicare and Medicaid, but there’s a lack of clarity as to whether it would impact other plans, such as exchange plans, where essential health benefits are required,” said Lindsey Dawson, director of LGBTQ Health Policy at KFF, the health policy research, polling, and news organization that includes KFF Health News.
State Medicaid programs vary widely in their rules around transgender care, with a variety of limits or restrictions on what types of care can be covered for minors in just over half the states, according to a map provided by the Colorado-based Movement Advancement Project, a nonprofit think tank.
While little is likely to happen immediately from the order — one of more than 100 issued by the president since his inauguration last week — it could, nonetheless, have a chilling effect on medical professionals.
The order directs the Department of Justice to work with Congress to promote legislation that would allow children and parents a “private right of action” — the ability to file a lawsuit — against medical professionals who provide transgender care.
And the Justice Department was also directed to consider the application of existing laws to those who provide or promote access to gender care.
In addition, one section of the order directs agencies to “take appropriate steps to ensure that institutions receiving Federal research or education grants end the chemical and surgical mutilation of children,” a move that could affect hospitals or medical schools.
Julian Polaris, a partner at the consulting firm Manatt, said the order “displays the federal government’s willingness to use federal programs to restrict access to disfavored services even to providers and patients outside those federal programs.”
The move drew immediate criticism from groups supporting LBGTQ+ people’s rights.
“It is unconscionable that less than 24 hours after trying to take away Head Start programs and school meals for kids, President Trump issued an order demonizing transgender youth and spreading dangerous lies about gender-affirming care,” Alexis McGill Johnson, president and CEO of Planned Parenthood Federation of America, wrote in a press release.
Because it defines “youths” as those under age 19, the order would apply the directives to medical treatments provided to 18-year-olds, who otherwise are considered adults in making legal choices, voting, or serving in the military.
“There’s also just a problem with not seeing young people as capable in making decisions around their health and their futures, and so blurring that line and trying to move it up and taking more control over more people is obviously concerning,” Ortiz said. “But having the line hard at 18 also doesn’t make it any better.”
Ortiz noted that the order contains misinformation about medical care for young people who are transitioning and targets a small subset of U.S. residents: transgender youths in families that can access and afford gender-affirming care.
“That should be concerning to everybody,” he said, “that they are pulling out populations to target, to say that, ‘We don’t think that you deserve access to best-practice medical care.'”
Trump’s order explained that the action was necessary because such medical treatment could cause young people to regret the move later, once they “grasp the horrifying tragedy that they will never be able to conceive children of their own or nurture their children through breastfeeding.”
KFF Health News Midwest correspondent Bram Sable-Smith contributed to this report.
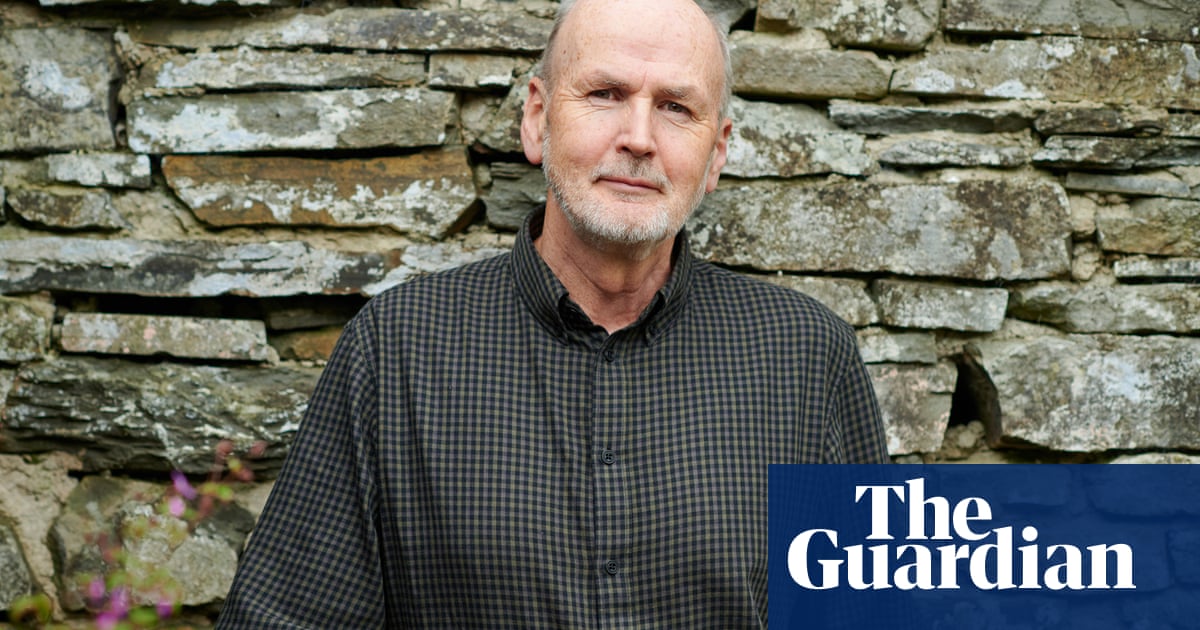
Niall Williams: ‘When I first read Chekhov, I thought: “He’s not so great”’ | Fiction
My earliest reading memory
I am sitting at the kitchen table at home in Dublin. I am home from school. I am in short pants; my legs dangle. The book in front of me is called Step By Step. It has no author. On the amber paper cover, in my mother’s handwriting, is my name. It is my first spelling book. I still have it. It begins with easy ones, No, Go, Soand works through 20 pages to Deck, Dock, Duck. Everything that follows begins here. When you know your spellings, it is a triumphant moment. You have been given a key.
My favourite book growing up
My hunger for books allowed no time for a favourite. I was on to the next one. All of Enid Blyton might be one multi-volumed book in my memory. The Famous Five and The Secret Seven and the Mystery series all passing through my hands in bedtime reading, to be replaced later by westerns, especially those of Louis L’Amour, whose great virtue was the supply would never run out, because he wrote so many.
The book that changed me as a teenager
Great Expectations by Charles Dickens. Mr Mason had us read it aloud in class, each of 30 teenage boys following the sentences with our finger. The world of that novel was more real to me than the one outside. When Pip fell in love with Estella, I did too.
The book that made me want to be a writer
I could say Dickens again here, for it seems to me that I began to write to rediscover the pleasure I had as a reader. But when I was 21, Christine Breen told me to read Gabriel García Márquez’s One Hundred Years of Solitude and when I emerged from the humid jungle of those pages, head spinning and imagination fevered, I knew that, for better or worse, making fiction was to be my life, and I hoped it would be with her.
The book or author I came back to
Chekhov. When I first read him as a teenager, I thought: “He’s not so great.” At that age I wanted style, brilliance, dazzlement. It took me 40 years to see his people, their profound humanness, and the genius of his story-making.
The book I reread
The Country Girls by Edna O’Brien. I read it first in university when I wanted to know what every famous Irish writer had done. I reread it when I was working on Time of the Child and realised that one of my characters, Ronnie, the doctor’s eldest daughter, who secretly wants to be a writer, was reading it. It is always startling when you find something is so much better than you remembered. I sent my salute to Edna at her extraordinary funeral.
The book I discovered later in life
I could make this plural and say everything by Edith Wharton. But in particular The House of Mirth. It was chosen by the book club that has met at our house for 16 years. During one year we read only “classics”, to see what that amounted to. And there was Edith, waiting.
The book I am currently reading
A Cold Eye: Notes from a Shared Island 1989-2024 by Carlo Gebler, with photographs by David Barker. Drawing on his meticulously kept journals from over 35 years, Carlo gives us one day for each year. In the company of these sharp, affectionate and wise entries you find yourself saying “Yes” often, and “God, I remember that.”
after newsletter promotion
